A new gene delivery platform promises to make cutting-edge cancer cell therapies faster, safer and more efficient, potentially widening patient access to life-saving treatments.
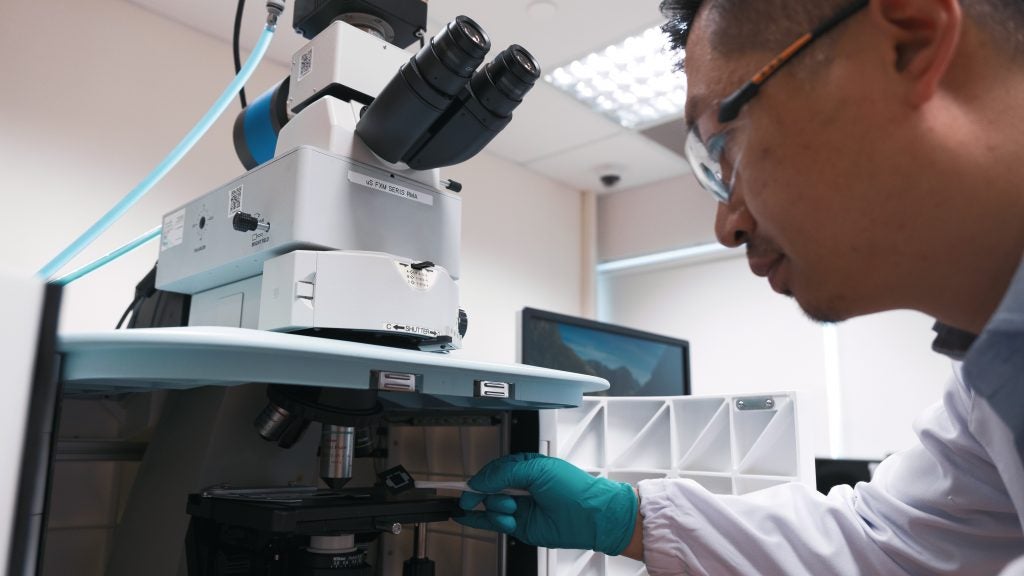
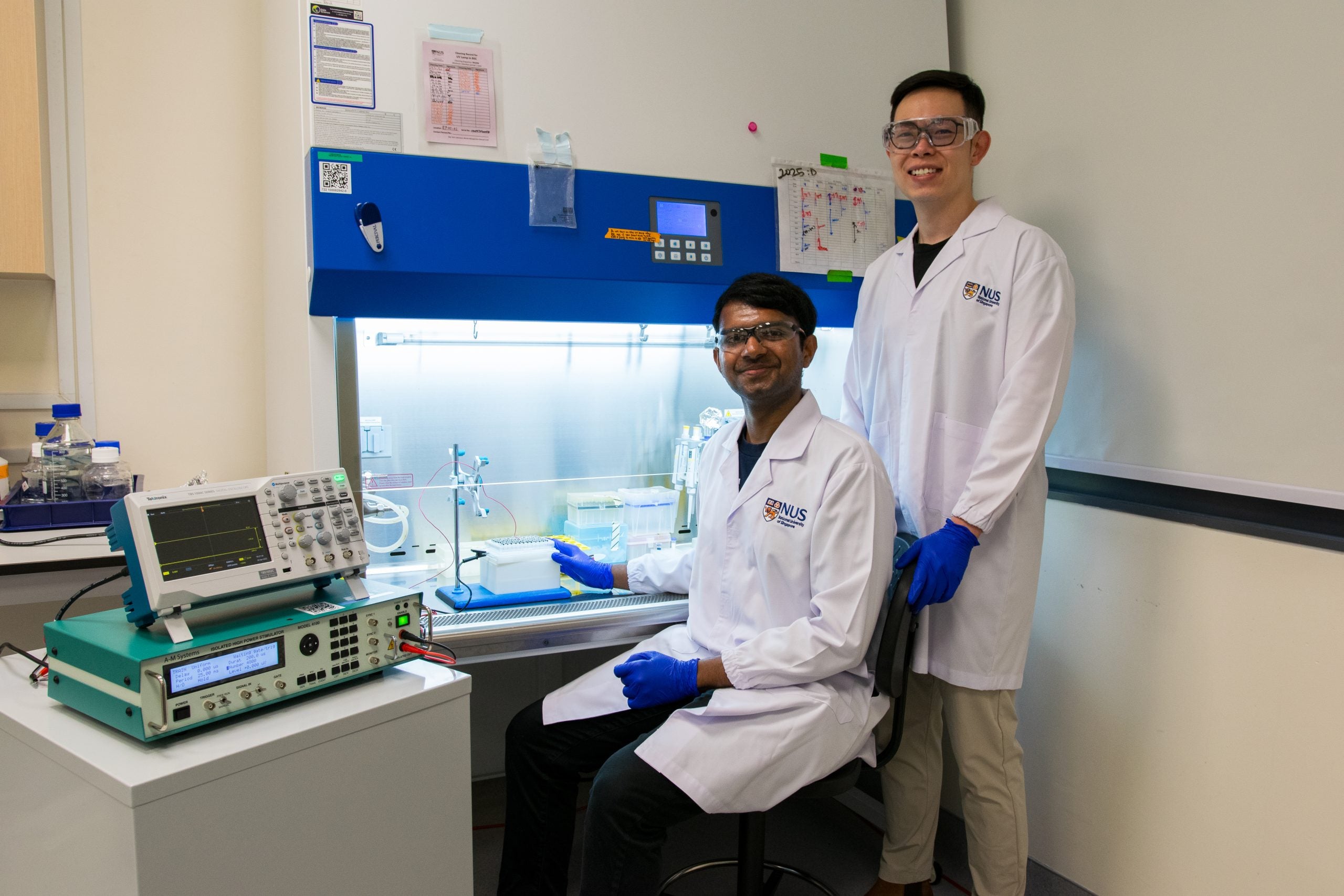
The non-viral system, known as Nanostraw Electro-actuated Transfection (NExT), has been developed by researchers led by Assistant Professor Andy Tay (Biomedical Engineering and the Institute for Health Innovation and Technology). It uses tiny hollow nanostructures and mild electrical pulses to deliver biomolecules — such as proteins, mRNA and gene-editing tools — into immune cells with high efficiency and minimal damage.
The researchers demonstrated that NExT can modify more than 14 million immune cells in a single run, including cell types that are typically difficult to engineer, such as gamma-delta T cells, T regulatory cells and natural killer cells.
The team’s findings were published earlier this year in the journal Biomaterials. Researchers from the NUS Yong Loo Lin School of Medicine also contributed to the study.
NExT makes gene delivery quicker and less damaging, which in turn helps lower manufacturing costs and improve the consistency of engineered cell products, including those used in chimeric antigen receptor-T (CAR-T) cell therapies for cancer. This could potentially widen patient access to advanced treatments that are currently limited by high costs and production challenges.
Next-generation gene delivery
Cancer remains one of the leading causes of death globally, responsible for nearly 10 million lives each year. Among the most promising treatment strategies to emerge in recent times is CAR-T cell therapy, which involves reprogramming a patient’s immune cells to recognise, target and kill cancer cells. This personalised approach has demonstrated success in treating blood cancers, especially in those who have exhausted conventional options. However, it remains expensive and logistically complex.
Last year the Singapore Ministry of Health began to provide subsidies for cell, tissue and gene therapy products (CTGTPs) that are assessed to be clinically and cost effective.The first CTGTP eligible for subsidy is a treatment known as tisagenlecleucel, a type of CAR-T cell therapy for treating blood cancers.
“In Singapore, a single CAR-T cell infusion can cost about S$670,000. Although subsidies are available, they typically cover only a fraction of the cost. This may limit access to the therapy for a significant number of patients, even as demand grows,” said Asst Prof Tay.
One of the main hurdles in CAR-T manufacturing lies in the delivery of genetic material into immune cells. Current industry-standard methods include viral vectors and bulk electroporation. On the one hand, while viral approaches are effective, they raise concerns around safety, immunogenicity and random gene integration. On the other, bulk electroporation, which relies on high-voltage electric pulses, can stress and damage cells, thus reducing their therapeutic quality.
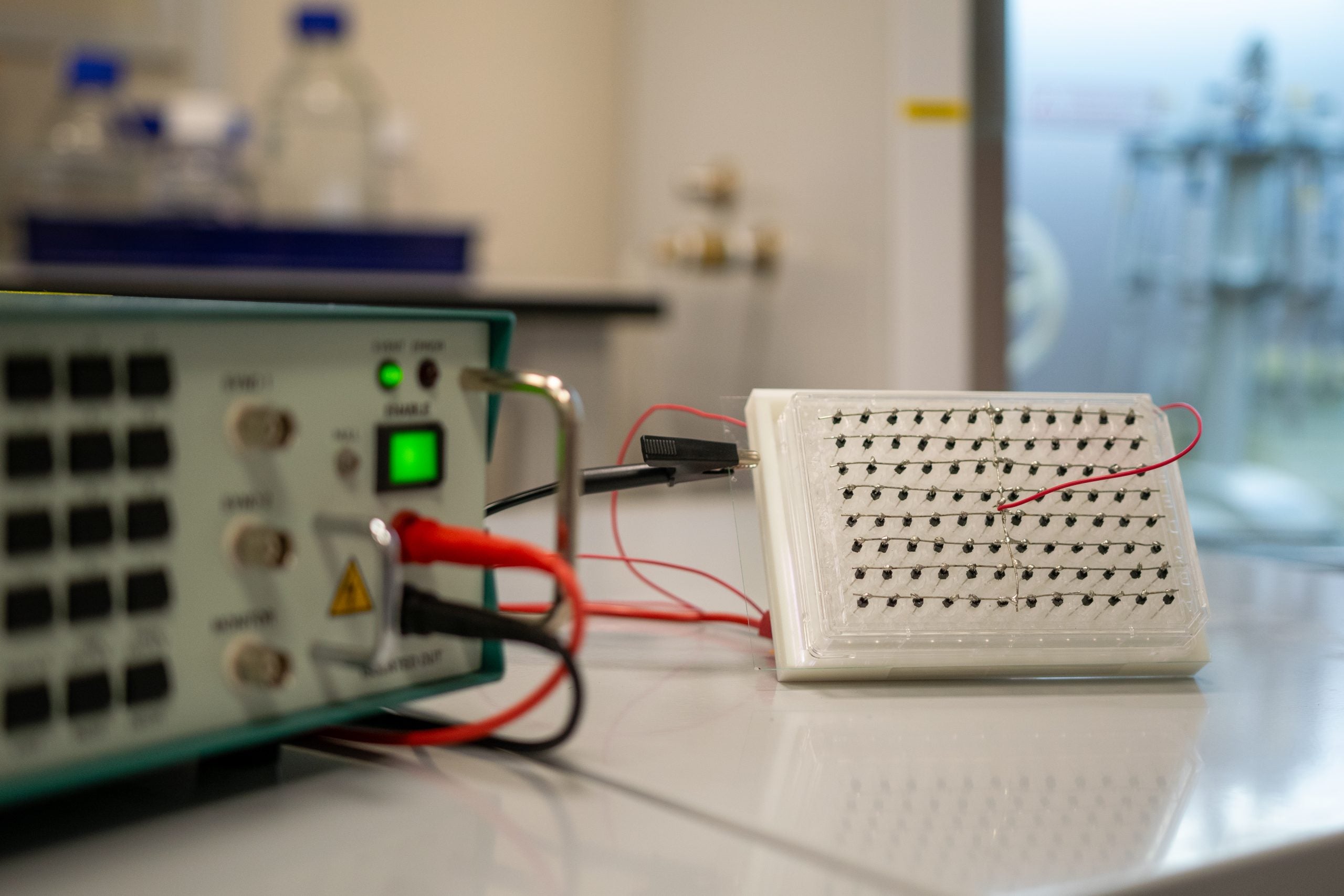
The NUS team’s NExT platform overcomes these limitations. It works by interfacing cells with a dense forest of nanostraws— microscopic hollow tubes less than a thousandth the width of a human hair. When a mild electrical signal is applied, the nanostraws open temporary pores in the cell membrane, allowing biomolecules such as mRNA or CRISPR/Cas9 complexes to enter the cell cytoplasm directly.
“Our NExT platform can handle a wide range of immune cell types. This is particularly timely as the field of cell therapy expands beyond traditional CAR-T approaches to include other cell types,” said Mr Arun Kumar, the paper’s first author and a PhD student at NUS supervised by Asst Prof Tay.
“Think of gene delivery like selecting a food delivery service. Ideally you want one that’s fast, reliable, keeps the food fresh and doesn’t cost a fortune. That’s what gene delivery should be like — efficient, cost-effective, doesn’t stress the cells too much, and adaptable to many different ‘orders’, or biomolecules,” added Mr Kumar.
In preclinical experiments, the NExT platform achieved transfection efficiencies of up to 94% for proteins and over 80% for mRNA in primary T cells, while maintaining key biological functions such as proliferation, migration and cytokine production.
“We were very encouraged to see that even after transfection, the immune cells retained their essential tumour-fighting characteristics. This suggests that the platform delivers both the efficiency as well as the cell quality needed for effective therapy,” said Asst Prof Tay.
More accessible and adaptable cancer treatments
The NExT platform can engineer alternative immune cells that are less likely to trigger severe immune reactions, and in some cases can function without matching the patient’s immune profile, making them suitable for “off-the-shelf” allogeneic therapies.
In addition, the high-throughput nature of the platform is designed to address the scale and cost bottlenecks of cell therapy production. The NUS researchers’ multi-well version of the platform can transfect over 14 million cells in a single run, enabling the simultaneous delivery of different genetic cargoes into multiple immune cell types from various donors to reduce production time.
Working towards clinical translation, the team’s next step is to validate the technology in preclinical studies before advancing to human trials. They are also working with industry partners to explore how the system can be integrated into existing cell therapy manufacturing workflows and are actively seeking opportunities to test the platform in real-world commercial settings