Women with heart valve disease may soon benefit from more targeted treatments, thanks to an AI-led study addressing long-standing gaps in cardiovascular drug development.
A team of international researchers co-led by Professor Dean Ho (Head, Department of Biomedical Engineering at CDE and Director of the Institute for Digital Medicine (WisDM) at NUS Medicine) and Professor Brian Aguado at the University of California, San Diego, has identified drug combinations tailored to the different ways men and women respond to aortic valve stenosis (AVS), a life-threatening heart condition common in older adults.
Their study was published recently in the journal Science Advances.
AVS affects about one in eight adults over 75 worldwide. It occurs when the heart’s aortic valve becomes stiff or narrowed, restricting blood flow and potentially leading to heart failure if left untreated. However, despite advances in medicine, most cardiovascular drugs have traditionally been tested mainly on men, often overlooking crucial biological differences between the sexes.
To tackle this, the research team used an AI-driven platform called IDentif.AI to screen 59 drug combinations on lab-grown heart valve cells derived from male and female models. This approach helped pinpoint which drug cocktails were most effective for each sex in preventing valve stiffening and scarring, the hallmarks of AVS progression.
“Men and women may need different medications to achieve the best outcomes,” said Prof Ho. “Using AI, we can identify these differences quickly and design personalised treatments that work better for everyone.”
The IDentif.AI platform revealed that male and female heart valve cells responded best to different drug combinations. Some cocktails worked well for female cells but were less effective in male cells, and vice versa. Some of the most promising combinations included Losartan, a common blood pressure medication. This suggests that combining existing approved drugs with experimental ones could speed up the development of new treatments for AVS.
Currently, the main treatment for AVS is surgical or transcatheter valve replacement, which carries risks especially for elderly patients. Sex-specific drug therapies could provide less invasive alternatives or delay the need for surgery.
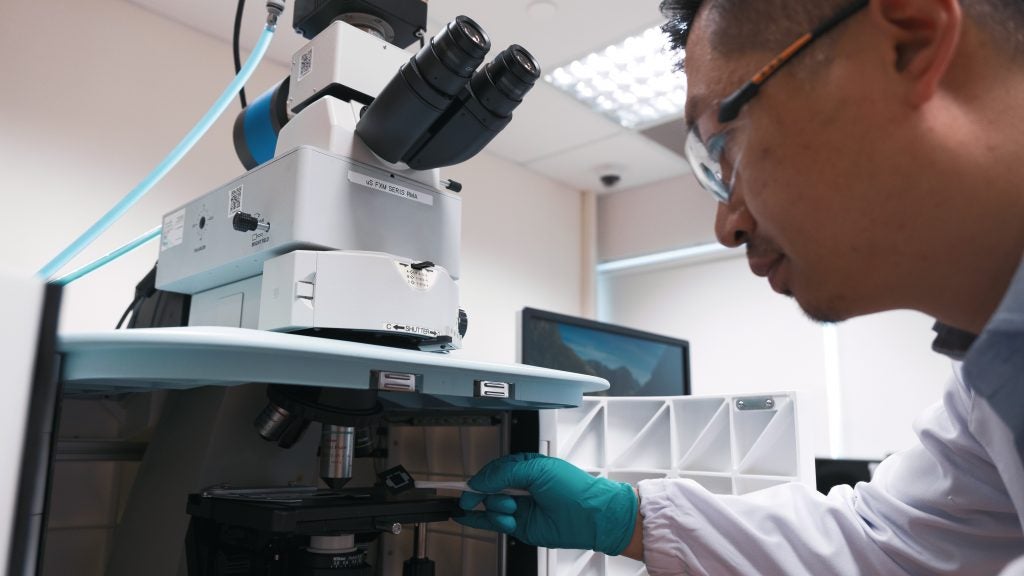
Dr Peter Wang, co-author from WisDM at NUS Medicine, highlighted the broader implications of the study: “We want to shift the conversation toward designing treatments that recognise how men and women respond differently to disease and medication,” he said. “Using the IDentif.AI platform is a step toward more personalised and more effective cardiovascular care.”
The research team plans to further test these AI-designed drug combinations in advanced laboratory models and explore their potential in other diseases with sex-specific treatment responses.