Keeping cancer cells content
Follow CDE
PDF Download
A jelly-like hydrogel platform keeps tumours alive for ten days, enabling an effective testing ground for various anti-cancer drugs and treatments.
Like our fingerprints, no two cancers are alike. Each individual cancer — even those of the same type — carries a myriad of genetic nuances, and may therefore behave differently and respond to treatments in distinct ways.
Recognising these subtleties has led to the advent of ‘personalised medicine’ in the medical lexicon. In this context, culturing fragments of a patient’s tumour can do wonders in pinpointing the most effective anti-cancer drugs for that particular individual. But once those cancer cells leave the body, a countdown begins. As clinical scientists race to decipher the molecular and cellular underpinnings during the drug testing process, they often struggle to outpace the rapid speed at which tumour tissue disintegrates.
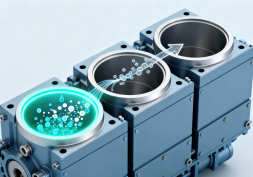
Assistant Professor Eliza Fong from the Department of Biomedical Engineering at the College of Design and Engineering, National University of Singapore, has a trick up her sleeve to ‘freeze’ those cells in time — using hydrogels. Functioning as scaffolds, these hydrogels contain structures that can hold the composition and architecture of the tumour fragments in place for ten days — well beyond the two-day window typically afforded.
This extended preservation allows scientists more time to study the tumour, figure out what drugs work best and ultimately save time, resources — and most importantly — lives.
Their findings were published in Biomaterials on 2 January 2024.
Assistant Professor Eliza Fong led research to pioneer the development of a hydrogel capable of prolonging the use of cancer cells for drug testing.
Turning the tide on time-limited processes
Unravelling cancers for drug testing is complex — riddled with its complicated webs of diverse cells, interactions and mechanisms that need to be uncovered. Examining tumour samples ex vivo, outside the patient’s body, is one effective way to study the disease in a controlled environment. Compared to traditional cancer cell cultures and organoid models, it better preserves the tumour’s natural architecture and cellular interactions, providing a more accurate model for testing treatments.
Nevertheless, the short lifespan of such samples limits their viability, putting a damper on comprehensive drug testing. To extend the lifespan of tumour samples, Asst Prof Fong led a team to bioengineer a jelly-like hydrogel made of hyaluronic acid, a water-based, lubricating fluid found naturally in the eyes and joints — and commonly used in skincare products as a moisturiser.
"We found that various biophysical properties, such as stiffness, degradability and integrin adhesivity, of the hydrogel matrix play an important role in maintaining the viability, tissue integrity and composition of the tumour slices."
"We found that various biophysical properties, such as stiffness, degradability and integrin adhesivity, of the hydrogel matrix play an important role in maintaining the viability, tissue integrity and composition of the tumour slices."
Using a vibrating microtome machine, the researchers shaved precise fragments of tumours taken from patients with head and neck cancers and cultivated them on the hydrogel.
“We found that various biophysical properties, such as stiffness, degradability and integrin adhesivity, of the hydrogel matrix play an important role in maintaining the viability, tissue integrity and composition of the tumour slices,” says Asst Prof Fong.
For instance, the stiffness of the matrix influences how well the cellular structures of the tumour are preserved. The hydrogel is also customisable to support the culturing of other cancers, such as such as peritoneal, lung, colorectal and ovarian. Samples from metastatic tumours, for instance, may require a hydrogel matrix that is less adhesive and more resilient to prevent cancer cells from invading and disrupting the matrix. On the other hand, matrices that are more porous can better facilitate the flow of nutrients and oxygen throughout the hydrogel, which in turn benefits tumours that are metabolically demanding and highly vascularised.
"We found that various biophysical properties, such as stiffness, degradability and integrin adhesivity, of the hydrogel matrix play an important role in maintaining the viability, tissue integrity and composition of the tumour slices."
“This can pave the way for longer-lasting hydrogel platforms tailored to each patient’s distinct tumour profile,” says Asst Prof Fong. “Think of them as true patient avatars for personalised and precision oncology!”
Conserving cellular chatter
When cancer cells are tightly packed together in a tumour, they can ‘talk’ to one another. This chatter also extends to neighbouring supporting cells. While these communication pathways facilitate tumour development and spread, decoding and targeting this cellular language can help turn the tables — halting its growth and averting drug resistance.
The team’s hydrogel preserves cell-to-cell communication networks within the tumour microenvironment, including those integral to immunotherapy — a targeted approach that involves boosting the body’s immune system to identify, intercept and eradicate cancer cells.
“By maintaining the compositional heterogeneity of the original tumours, including various cell populations and their interactions, the hydrogel keeps crucial communication pathways intact,” says Asst Prof Fong. “This includes those related to immune checkpoint inhibitors (ICIs), a type of immunotherapy that puts the brakes on the cancer’s ability to evade the immune system, giving it a fighting chance to attack cancer cells more effectively.”
Co-clinical trial results have revealed that cancer cultures preserved in the hydrogel may indeed predict sensitivity to ICIs in head and neck cancer patients. “This is an exciting development as it suggests that our hydrogel can provide a more reliable method for evaluating patient-specific responses to immunotherapy, potentially leading to more individualised treatments.”
At the frontiers of cancer treatment
While promising, the researchers point out that there are still limitations in predicting immune responses in metastatic or recurrent tumours, which may differ from the original resected tumour.
Further research is underway to clinically validate how the team’s hydrogel responds in larger patient populations. The researchers also suggest exploring the inclusion of perfusion to preserve vasculature and the integration of tumour-draining lymph nodes to enhance the accuracy of ICI efficacy predictions — all of which could expand the applications of their groundbreaking hydrogel platform.
Read More
View Our Publications ▏Back to Forging New Frontiers - July 2024 Issue
If you are interested to connect with us, email us at cdenews@nus.edu.sg