A wearable sensor that enables the continuous detection of key health biomarkers directly from the patient’s skin could mark a major step forward for real-time personalised healthcare and early detection of diseases.
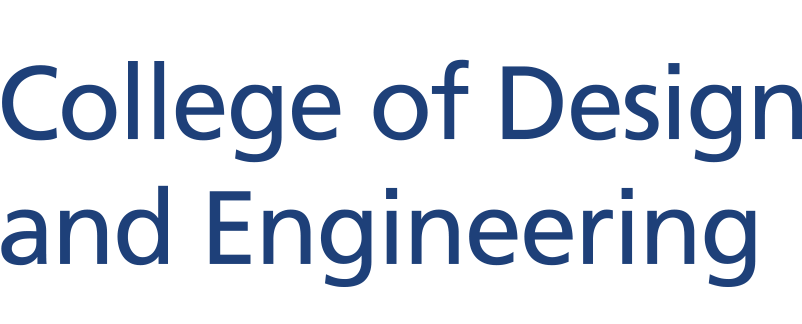
The device, developed by a team led by Assistant Professor Liu Yuxin (Biomedical Engineering), promises a convenient alternative to many tedious and sometimes painful monitoring methods such as blood draws and urine tests. According to the research team, the new sensor has a wide range of applications including chronic disease management, population-wide screening, and remote patient monitoring - for example, with diabetic patients.
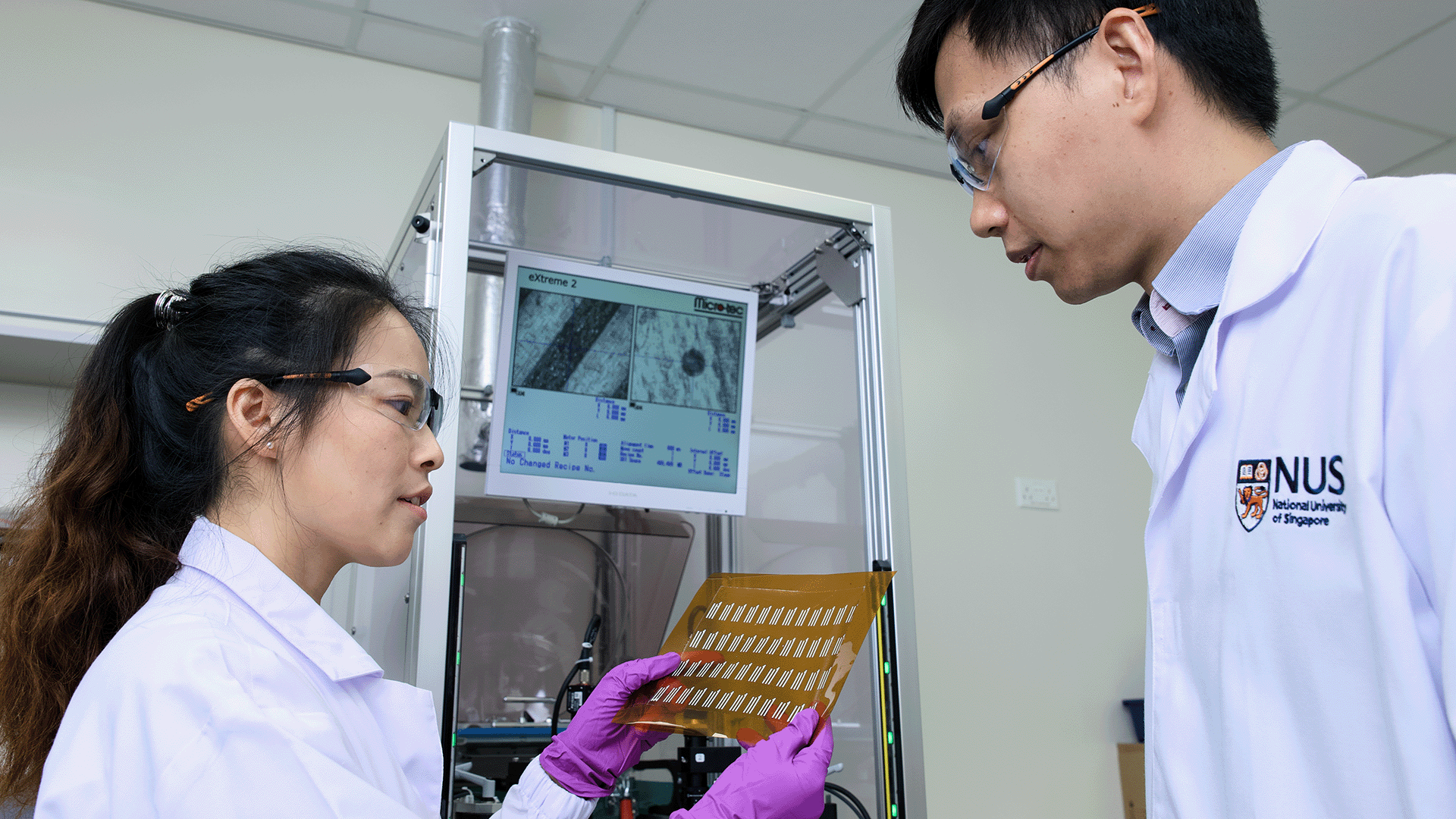
The research study which developed the sensor is a collaboration with Dr Yang Le from the Agency for Science, Technology and Research (A*STAR). The team’s findings were published recently in the journal Nature Materials.
“Monitoring health markers — molecules found in blood and other body fluids that show what's happening in your body — usually involves testing blood, urine, or sweat,” said Asst Prof Liu, who is also with the NUS Institute for Health Innovation & Technology as well as N.1 Institute for Health. “However, blood tests are invasive, inconvenient and sometimes painful, urine tests can be a hassle and don't provide immediate results, and sweat tests are tricky because it's hard to make people sweat without exercise or using uncomfortable sweat-inducing drugs. These issues make it harder to detect diseases early and start treatment promptly.”
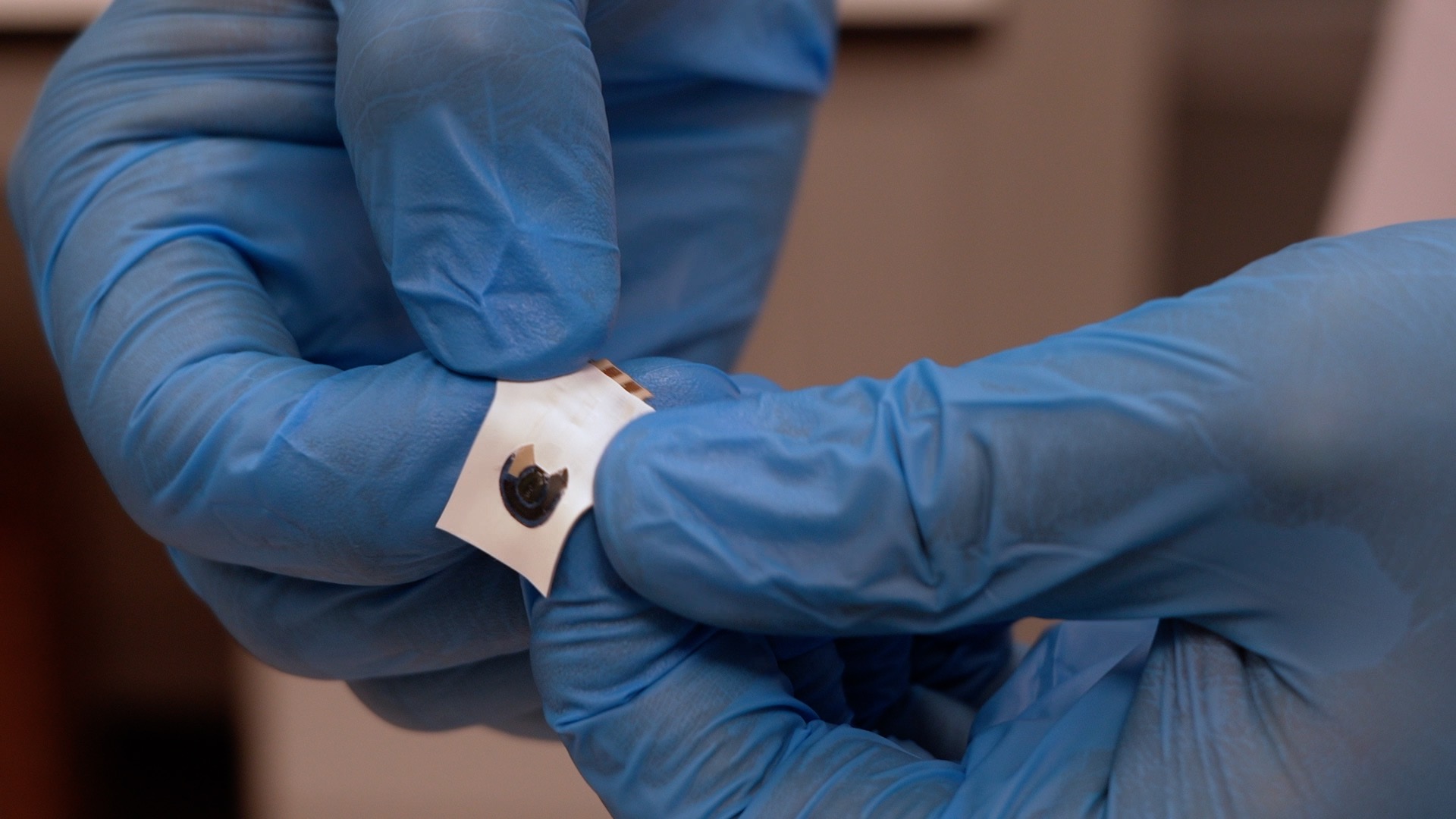
With this in mind, the new sensor has been designed to detect solid-state epidermal biomarkers (SEBs) directly from a patient’s skin. These markers, like cholesterol, lactate, and glucose, are found in the outer layer of the skin and are linked to diseases like heart disease and diabetes. However, until now it has been hard to detect these markers directly on the skin because traditional methods don't work well with solid-state markers.
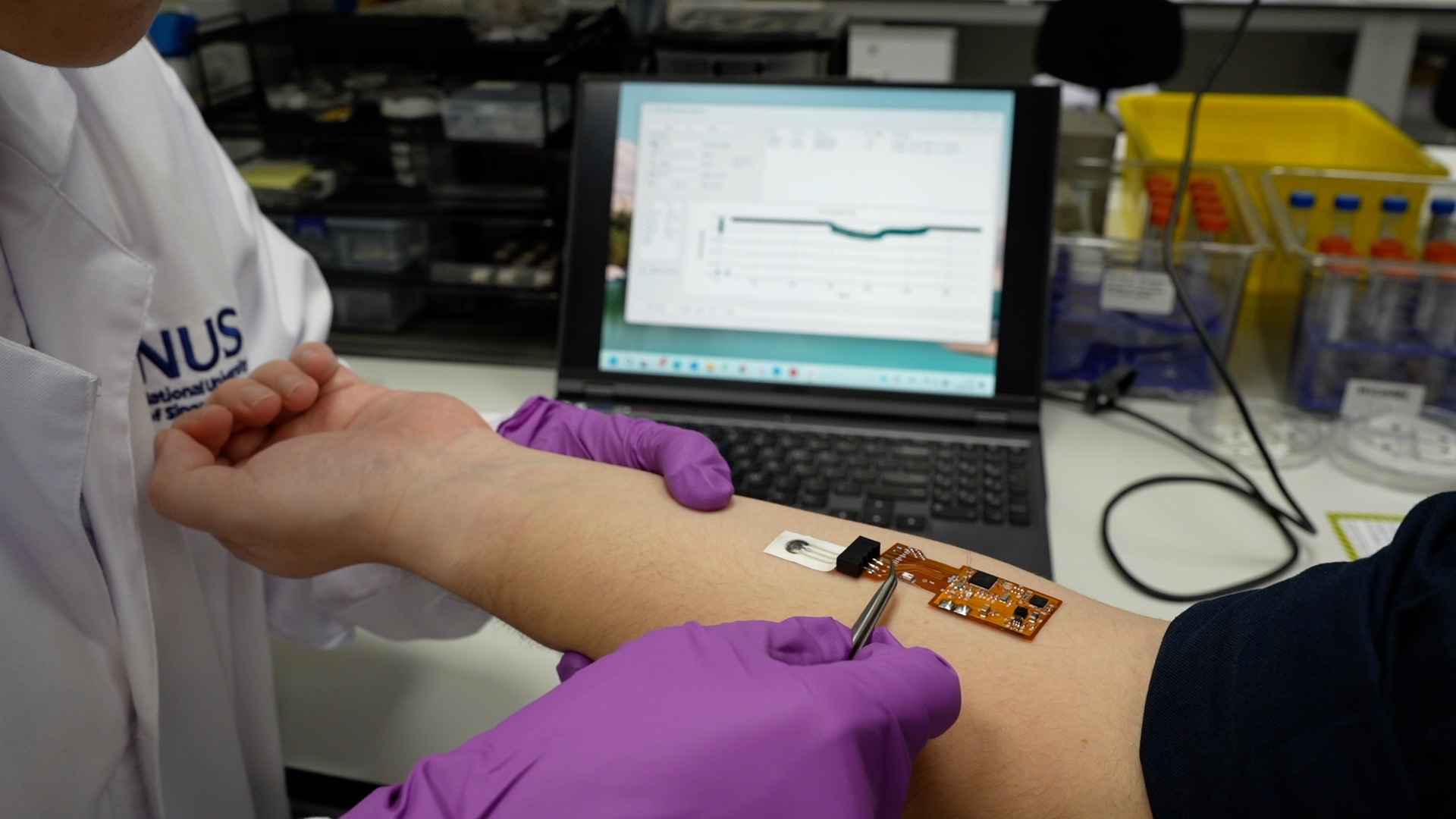
Asst Prof Liu’s team solved this problem with an innovative two-layer, hydrogel-based SEB sensor. One layer of the sensor dissolves the markers from the skin, and the other layer helps translate the information into an electrical signal. The sensor and its attached circuit board have been designed to be flexible and waterproof, meaning they can easily be worn without discomfort or interfering with the wearer’s daily activities.
“When you wear the sensor, the markers dissolve into the first layer, move through the hydrogel, and react with enzymes,” said Asst Prof Liu. “The SEB sensor then sends the health data wirelessly using a Bluetooth signal to an external device, giving you continuous updates on your health.”
In clinical studies, the SEB sensor showed that the health markers it detected on the skin were comparable to those found in traditional blood tests. This proves the sensor's accuracy and suggests it could replace blood tests for monitoring chronic diseases like diabetes and heart conditions.
“The SEB sensor is also very sensitive, with an ability to detect even extremely low amounts of lactate and cholesterol," said Asst Prof Liu. "This makes it as precise as advanced lab equipment."
The sensor's flexible, skin-like design also reduces errors caused by the wearer’s movements. Traditional sensors can be affected by how they are placed on the skin or by the users moving around, but the new sensor is three times better at handling these issues. This improvement was confirmed through mathematical modelling undertaken by co-researchers Dr Liu Zhuangjian and Dr Li Hongying at A*STAR.
Moving forward, the research team plans to improve the SEB sensor's performance by increasing its working time and sensitivity. They also want to add more health markers to the sensor, making it useful for a wider range of conditions.
“We’re working with hospitals to test the SEB sensor further and bring it to patients, especially for continuous glucose monitoring,” said Asst Prof Liu. “We hope to have the sensor available commercially in about five years.”